ANATOMY OF THE GALL BLADDER AND BILE DUCTS
Gall bladder is a pear or globular shaped organ present in the right hypochondrium on the inferior surface of the liver, situated in the gall bladder fossa. It is about 8-12 cm long.
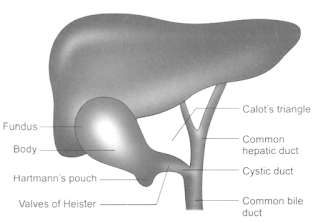
• Fundus: It is the dilated portion of the gal !bladder adherent to undersurface of liver from which it can be separated easily.
• Neck: The narrow angulated distal portion of the neck is called Hartmann 's pouch-common site where stones occur and tend to stay for a long time (also called infundibulum of gall bladder).
• Gall bladder drains into the common bile duct (CBD) through cystic duct, which is 3 cm long. It is lined by cuboidal epithelium. There are prominent mucosal folds within the cystic duct due to the presence of prominent circular muscle fibres underneath. Its lumen is usually 1-3 mm in diameter. Contraction of gall bladder produces a functional valve called valve of Heister which prevents the migration of stone into the CBD. The wall of cystic duct issurrounded by a sphincter structure called sphincter of Lutkens. A spiral fold keeps cystic duct open for drainage of bile.
Cholecystohepatic triangle or Calot's triangle boundaries
• Lateral: Cystic duct and gall bladder
• Medial: Common hepatic duct
• Above: Inferior surface of right lobe of the liver.
It is an important landmark in the identification of cystic duct, and cystic artery during cholecystostomy so as to avoid damage to extrahepatic biliary tree.
Contents
• Right hepatic artery and its branch, the cystic artery
• Cystic lymph node of Lund.
Blood supply of gall bladder
Cystic artery, a branch of right hepatic artery arises behind the common bile duct. Soon, it branches out over the surface of gall bladder. Cystic artery is an end artery.
Multiple small veins from the surface of gall bladder join the liver surface. There is also a cystic vein, from the neck of gall bladder draining into portal vein directly. This explains early spread of gall bladder malignancy to the liver.
Lymphatics
1. Subserosal and submucosal lymph nodes drain into cystic lymph node of Lund and from here they drain into nodes in the hilum of liver and coeliac nodes.
2. Subserosal lymphatic vessels of gall bladder are also connected to subcapsular lymph channels of liver, which accounts for frequent spread of carcinoma gall bladder to the liver.
Anatomy of the bile ducts
• Common hepatic duct (CHD) is formed by the union of right and left hepatic ducts. It is 3 cm long, receives cystic duct and continues as common bile duct (CBD).
• Common bile duct is about 8 cm long. It has four parts: Supraduodenal, retroduodenal, infraduodenal and intraduodenal. Along with pancreatic duct, it forms ampulla of Yater. Controlled by sphincter of Oddi, it ends by an opening into the second part of duodenum.
Functions of the gall bladder
• Reservoir for bile: Bile excreted by the liver is stored in the gall bladder as total of about 500 to 1000 ml per day. At fasting, the tone of sphincter of Oddi is high. Food contents in the duodenum stimulates release of cholecystokinin, which causes gall bladder to contract.
• Concentration: Bile is 98% water. Due to active absorption of water, sodium chloride and bicarbonate, bile gets concentrated 5-10 times. Thus, a relative increase in bile salts, bile pigments, cholesterol and calcium occurs.
• Mucus secretion: It secretes about 20 ml/mucus per day.Obstruction to the cystic duct causes mucocoele of the gall bladder.
Bile
• Secreted from hepatocytes
• pH is more than 7.0
• 500-1000 ml/day, 98% is water
• Concentrated in gall bladder because of absorption of water. Capacity of gall bladder is 40-50 ml.
• Fatty food stimulation releases cholecystokinin, which stimulates gall bladder to contract and at the same time, sphincter of Oddi to relax.
•It also has inorganic ions (more than plasma) and hence, severe electrolyte imbalance is seen in biliary fistula.
• Cholesterol, synthesised in the liver, gives rise to bile acids-cholic and chenodeoxycholic acids. They are metabolised in the colon to deoxycholic acid and lithocholic acids.
• Main function of bile acids in the bile is to maintain cholesterol in solution.
CONGENITAL ANOMALIES OF GALL BLADDER
Absence of gall bladder: Very rare; other variations include
A. Floating gall bladder: Results due to long mesentery. It is more vulnerable to torsion-a rare cause of recurrent upper abdominal pain. Such a gall bladder can be easily removed.
B. Phrygian cap: Cap which was worn by people of Phrygia (ancient Asian country, Mongolia). It is an anomaly connected with the fund us of the gall bladder.
C. Double gall bladder: The second one is always intrahepatic (rare).
D. Absence of cystic duct: Cholecystectomy becomes difficult. There are high chances of injury to the common bile duct.
E. Low insertion of cystic duct: Cystic duct opens into the common bile duct near the ampulla. This anomaly should be kept in mind when operating on cases of obstructive jaundice.
F. An accessory or aberrant cholecystohepatic duct present in about I 0% of the patients. It may be the cause ofsignificant bile leakage after cholecystectomy. It is the segmental duct that joins biliary system outside the liver instead of within it.
G. Diverticulum of gall bladder
H. Cystic duct joining right hepatic duct.








No comments:
Post a Comment
please do not enter any spam link in the comment box